This article may contain references to products or services from one or more of our advertisers or partners. We may receive compensation when you click on links to those products or services. Nonetheless, our opinions are our own.
The information presented in this article is accurate to the best of our knowledge at the time of publication. However, information is subject to change, and no guarantees are made about the continued accuracy or completeness of this content after its publication date.
- Navigating Health Insurance
- Understanding Your Healthcare Needs
- Evaluating Coverage Options and In-Network Providers
- Assessing Premiums, Copays, and Deductibles
- Exploring Additional Benefits and Perks
- Comparing Prescription Drug Coverage
- Choosing the Best Option: Tips for Selecting the Right Plan
- How to Select a Health Insurance Marketplace Plan
- Things to Consider When Choosing Plans in the Health Insurance Marketplace
- Estimating Your Total Healthcare Costs
- Understanding Total Costs Beyond Premiums
- Evaluating Health Insurance Plan Types
- Comparing HMO, PPO, EPO, and POS Plans
- Conclusion
- Frequently Asked Questions
- Recommended Reads
Navigating health insurance can be challenging due to the numerous options available. Whether you’re selecting a plan for the first time or considering a change, understanding how to compare health insurance plans is crucial for making an informed decision. Many people feel overwhelmed by the details and terminology—but you’re not alone.
This guide will walk you through the most important factors to consider, including monthly premiums, deductibles, copayments, and provider networks. By the end, you’ll feel confident in reviewing your options and selecting a plan that fits both your health needs and your budget.
Understanding Your Healthcare Needs
When evaluating health insurance plans, it’s crucial to assess your personal and family healthcare needs. This helps narrow down the choices and identify the plans that best support your lifestyle. Key factors to consider include
Your Health Status
Think about any chronic conditions, recent illnesses, or ongoing treatments that require regular care or specialist visits.
Family Needs
If you’re responsible for others—such as children or a spouse—consider their medical needs, including pediatric care or specialist services.
Budget
Review your income and expenses to determine what you can reasonably afford to spend on premiums, deductibles, and copays.
Preferred Providers
List your current doctors, specialists, and hospitals. Check whether they’re part of the networks of the plans you’re considering.
Creating a comparison table is a great way to organize your thoughts.
| Plan Name | Monthly Premium | Deductible | Out-of-Pocket Max | In-Network Coverage |
|---|---|---|---|---|
| Plan A | $400 | $1,500 | $6,000 | 80% |
| Plan B | $350 | $1,000 | $5,500 | 90% |
This helps you visualize which plan aligns best with your needs and financial situation.
Evaluating Coverage Options and In-Network Providers
Understanding what services are covered—and at what cost—is essential for choosing the right plan. Here are important coverage areas to look at:
Essential Health Benefits
Verify that the plan includes essential services such as emergency care, hospitalization, maternity care, and mental health services.
Preventive Services
Look for plans that offer free or low-cost preventive care, such as annual check-ups, screenings, and vaccinations.
Prescription Medications
Make sure your regular prescriptions are included in the plan’s drug list, and review the out-of-pocket costs for each tier.
In-network providers are another crucial factor. Each plan has a network of providers who agree to offer services at reduced costs. Things to evaluate:
Availability
Ensure your preferred doctors are in-network and accepting new patients.
Quality of Care
Review provider ratings and patient feedback when possible.
Convenience
Factor in location and appointment availability.
| Plan Type | In-Network Coverage | Out-of-Pocket Costs |
|---|---|---|
| HMO | Requires referrals | Lower costs |
| PPO | Flexible choice | Higher costs |
| EPO | No referrals required | Moderate costs |
Carefully reviewing provider access and service availability can help you avoid unexpected costs and maintain continuity of care.
Three of the most important financial terms to understand are
The monthly cost you pay to keep your insurance active. Lower premiums can be appealing but may come with higher out-of-pocket expenses.
Copay
A fixed fee you pay for specific services (e.g., $30 for a doctor’s visit).
Deductible
The amount you pay out of pocket before your insurance begins covering services. Higher deductibles usually mean lower premiums.
Here’s a table to illustrate the differences:
| Plan | Monthly Premium | Deductible | Copay (Doctor Visit) |
|---|---|---|---|
| Plan A | $300 | $1,500 | $30 |
| Plan B | $250 | $2,000 | $20 |
| Plan C | $400 | $1,000 | $40 |
Choose a plan based on how often you expect to use medical services and your ability to cover upfront costs.
Exploring Additional Benefits and Perks
Beyond the basics, many plans offer valuable extras that can improve your overall experience:
Preventive Services
Look for plans that cover vaccines, wellness exams, and screenings at no additional cost.
Wellness Programs
These may include discounts on gym memberships, nutrition counseling, and stress-reduction programs.
Telehealth Services
Virtual visits can save time and money, especially for routine care or mental health support.
Drug Discounts
Some plans provide discounts on prescription medications or access to lower-cost generic options.
Spending Accounts
Options like Health Savings Accounts (HSAs) or Flexible Spending Accounts (FSAs) allow you to set aside pre-tax money for qualified medical expenses.
Here’s a quick benefits summary:
| Benefit | Description |
|---|---|
| Virtual Care | Video or phone consultations with healthcare providers |
| Dental & Vision | Assistance with exams, glasses, and dental work |
| Health Savings Account | Pre-tax savings for healthcare-related expenses |
These perks can offer substantial savings and enhance the overall value of your plan.
Comparing Prescription Drug Coverage
Prescription costs vary widely, so it’s important to compare how each plan handles medications:
Cost Sharing
Understand what you’ll pay in copayments or coinsurance for different drug tiers.
Pharmacy Network
Confirm that your preferred pharmacies are in-network.
Check if certain medications require approval before coverage applies.
Mail-Order Benefits
Some plans offer savings for 90-day supplies of maintenance medications via mail.
Comparison example:
| Feature | Plan A | Plan B |
|---|---|---|
| Tier 1 Copay | $5 | $10 |
| Tier 2 Copay | $20 | $30 |
| Mail-Order Savings | Yes | No |
| Prior Authorization | Required | Not required |
Evaluating these details can help you avoid unexpected pharmacy costs.
Voted "Best Overall Budgeting App" by Forbes and WSJ
Monarch Money helps you budget, track spending, set goals, and plan your financial future—all in one app.
Get 50% OFF your first year with code MONARCHVIP
Choosing the Best Option: Tips for Selecting the Right Plan
If you’re still unsure, use these practical tips to help make your final decision:
Understand Your Needs
Consider your medical history, expected visits, and regular prescriptions.
Compare Total Costs
Don’t focus only on premiums—factor in deductibles, copays, and the out-of-pocket maximum.
Verify Provider Network
Make sure your preferred healthcare professionals and facilities are included.
Review Extra Benefits
Programs like telehealth or fitness incentives can make one plan stand out.
Example comparison:
| Feature | Plan A | Plan B |
|---|---|---|
| Monthly Premium | $200 | $180 |
| Annual Deductible | $1,500 | $1,000 |
| Out-of-Pocket Max | $5,000 | $7,000 |
| Preventive Care | Covered 100% | $30 Copay |
Creating a side-by-side comparison can make your choice easier and more informed.
How to Select a Health Insurance Marketplace Plan
When buying insurance through the Health Insurance Marketplace, consider plan categories (Bronze, Silver, Gold, Platinum), available subsidies, and your eligibility for cost-sharing reductions. The Marketplace is a good option for individuals, freelancers, and small business owners who do not have employer-provided coverage.
Things to Consider When Choosing Plans in the Health Insurance Marketplace
- Do you qualify for a premium tax credit or cost-sharing reductions?
- Are your preferred doctors and medications covered?
- How much do you expect to spend annually on healthcare?
Compare plans with both short-term costs (monthly premiums) and long-term expenses (deductibles and out-of-pocket maximums) in mind.
Estimating Your Total Healthcare Costs
Think beyond premiums. Include expected costs for:
- Regular doctor visits
- Specialist appointments
- Prescription drugs
- Potential emergencies or surgeries
Use your health history and planned procedures to estimate your total annual cost more accurately.
- Total costs = Premium + Deductible + Copayments + Coinsurance + Out-of-Pocket Max
- Don’t just choose the lowest premium—assess your total financial exposure.
Evaluating Health Insurance Plan Types
Each type of plan works differently in terms of provider access and costs.
Comparing HMO, PPO, EPO, and POS Plans
| Plan Type | Referrals Required | Out-of-Network Coverage | Cost Efficiency | Flexibility |
|---|---|---|---|---|
| HMO | Yes | No | High (Low Cost) | Low |
| PPO | No | Yes | Medium | High |
| EPO | No | No | High | Medium |
| POS | Yes | Yes (with referral) | Medium | Medium |
Choose the plan type that best matches your need for flexibility, cost savings, and preferred providers.
Conclusion
Selecting a health insurance plan is a crucial decision that impacts both your health and finances. Take time to consider your medical needs, review the total costs, and ensure your providers are in-network. Look for plans that offer valuable benefits, such as wellness programs or telehealth access.
Though it might feel overwhelming, breaking it down into manageable parts—and using tables and comparison tools—can simplify the process. When you understand your options, you can choose with confidence and peace of mind.
Frequently Asked Questions
Why is it important to compare health insurance plans?
Comparing plans helps you find the best fit for your needs and budget. Each plan varies in coverage, cost, and provider access.
What should I consider when comparing plans?
Focus on premiums, deductibles, copays, out-of-pocket limits, provider networks, and services offered.
How can I know if a plan meets my healthcare needs?
Review the plan’s Summary of Benefits and Coverage (SBC) or contact the insurer directly to ask questions.
What’s the difference between in-network and out-of-network?
In-network providers contract with your insurer and typically cost less. Out-of-network services may cost significantly more or not be covered at all.

Reviewed and edited by Albert Fang.
See a typo or want to suggest an edit/revision to the content? Use the contact us form to provide feedback.
At FangWallet, we value editorial integrity and open collaboration in curating quality content for readers to enjoy. Much appreciated for the assist.
Did you like our article and find it insightful? We encourage sharing the article link with family and friends to benefit as well - better yet, sharing on social media. Thank you for the support! 🍉
Article Title: How to Compare Health Insurance Plans for the Best Coverage
https://fangwallet.com/2025/04/24/compare-health-insurance-plans/The FangWallet Promise
FangWallet is an editorially independent resource - founded on breaking down challenging financial concepts for anyone to understand since 2014. While we adhere to editorial integrity, note that this post may contain references to products from our partners.
The FangWallet promise is always to have your best interest in mind and be transparent and honest about the financial picture.
Become an Insider
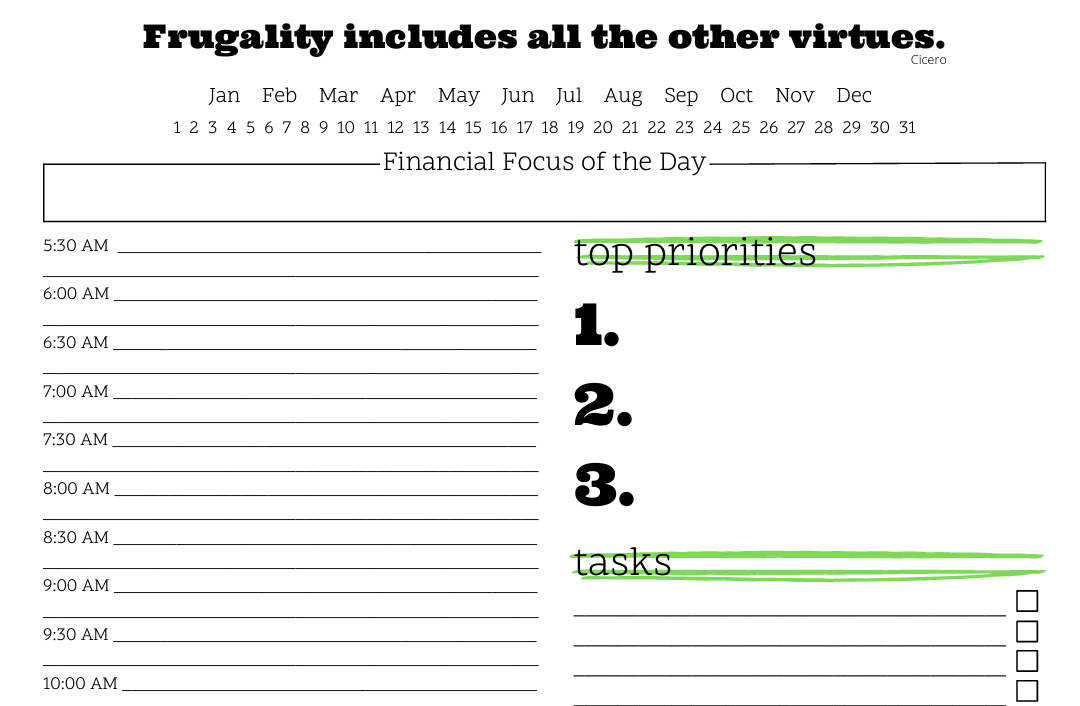
Subscribe to get a free daily budget planner printable to help get your money on track!
Make passive money the right way. No spam.
Editorial Disclaimer: The editorial content on this page is not provided by any of the companies mentioned. The opinions expressed here are the author's alone.
The content of this website is for informational purposes only and does not represent investment advice, or an offer or solicitation to buy or sell any security, investment, or product. Investors are encouraged to do their own due diligence, and, if necessary, consult professional advising before making any investment decisions. Investing involves a high degree of risk, and financial losses may occur including the potential loss of principal.
Source Citation References:
+ Inspo
There are no additional citations or references to note for this article at this time.